Maintaining surgical instruments is critical for patient safety, such as avoiding infections and tissue damage, and for the longevity of these tools. However, common mistakes like improper cleaning, skipping lubrication, or using instruments for unintended purposes can lead to corrosion and malfunctioning, and put patients at risk. Even disposable instruments must be used following the guidelines and, of course, disposed of properly.
Surgeons and those who supply their tools must understand these pitfalls to ensure optimal performance and safety. This article explores some of the most dangerous maintenance mistakes and how to avoid them to keep surgical tools in top condition.
Incorrect cleaning methods
Incorrect or improper cleaning of reusable surgical instruments is one of the leading causes of ineffective sterilization. Ineffective sterilization, in turn, is an important risk factor for the development of nosocomial infections.
Unclean surgical instruments may result from not following standard cleaning procedures or choosing an incorrect cleaning method. A study analyzing the factors behind device cleaning quality found the main reason for cleaning failures was the cleaning personnel’s practice of ignoring standard procedures to save time.
The study authors recommend creating workflow charts and diagrams that clearly illustrate the disassembly and cleaning procedures for different surgical instruments to prevent cleaning-related mistakes. For example, instruments with power systems and precision ophthalmic devices require combined manual washing-off of contaminants with water and ultrasonic cleaning. In contrast, lumen devices require cleaning with a pulsating vacuum.
Comprehensive guidelines, such as the recommendations by the Robert Koch Institute in Germany, precisely define the standard of cleaning surgical instruments and other medical devices.
Improper storage
Improperly storing surgical instruments is another cause of instrument contamination that puts the patient’s safety at risk.
Sterilized surgical instruments are usually packed or wrapped before storage. However, a mishandling of the instruments may lead to tears, wet wrapping, abrasions, or unsecured wrapping, thus compromising the sterility of the instruments. Moreover, this mistake leads to the need for instrument re-sterilization, which causes surgery delays.

The instrument storage area should be dry and clean. Prominent organizations, such as the Royal Australian College of General Practitioners (RACGP), have listed guidelines on storing sterilized reusable surgical instruments. The Joint Commission also offers a set of standards for using ventilator equipment to regulate the temperature and humidity of the device storage area. According to these standards, the relative humidity in the storage area should not exceed 60%, while the temperature should be 22–26°C (72–78°F).
Not following sterilization protocols
Surgical instrument sterilization is the process of destroying all microorganisms on the surface of the instrument. It includes autoclaving (steam sterilization), chemical sterilization, dry heat sterilization, etc.
Sterilization protocols, however, are guidelines that professional organizations in healthcare publish and update regularly. An example of a sterilization protocol is the Guideline for Disinfection and Sterilization in Healthcare Facilities (PDF) from the U.S. Centers for Disease Control and Prevention (CDC).

According to the CDC, using inadequately sterilized instruments and devices represents a high risk of transmitting infectious microorganisms. However, despite the risk, the documented transmission of pathogens from improperly sterilized items is exceedingly rare. An explanation for this counterintuitive fact is the wide margin of safety of sterilization processes used in healthcare.
Improper handling during procedures
Handling a surgical instrument is an art; it requires practice, knowledge, and an eye for precision. The sterilization staff, operating room nurses, and surgeons are all responsible for correctly handling before, during, and after surgeries.
During surgery, surgeons and nurses must use the instruments only according to the manufacturer’s instructions. They must be aware of the number and location of the instruments and pay attention when passing them over to one another. Handling-related mistakes during surgery may damage the instruments and risk the patient’s health. Specialized tools, such as magnetic instrument trays, effectively help prevent accidents associated with instrument handling by keeping the instruments in place when they’re not in use.
Before and after surgery, the sterilization team must ensure that surgical instruments are handled adequately during sterilization, cleaning, transportation, and storage procedures. Any mistake during these stages forces a complete “redo” of the instrument maintenance steps, wasting time and resources and shortening the instruments’ lifespan.
Using instruments for unintended purposes
Each surgical instrument serves a particular function that complements the function of other instruments during surgery. Forceps are typically applied to hold tissues apart while a blade easily cuts through soft tissues.
Occasionally, the operating room staff might “improvise” by using an instrument to perform a purpose other than the one determined by its manufacturer. For example, the staff might use clamps to hold surgical drapes in place. This practice can lead to frequent instrument use and premature wear.
To avoid unintended use and potential damage, hospitals must strive to train all personnel on the correct application of each instrument type based on the manufacturer’s directions.
Not lubricating hinged instruments
Hinged instruments are open-close hinge mechanisms, such as scissors, needle holders, or artery forceps. Surgical lubricants, such as Surgilube® and lignocaine cream, are jelly-like substances that can be applied to hinged instruments to prevent corrosion and stiff joints. Not lubricating hinged instruments leads to premature corrosion and stiffness that compromise the function of the instrument.

The sterile department staff may apply a lubricant to hinged instruments immediately after cleaning them. A water-based synthetic lubricant is preferred to an oil-based lubricant, as the latter can prevent proper sterilization. If water-based lubricants are unavailable, the staff can use ordinary sewing machine oil or hot, clean water.
Not following manufacturer guidelines
Every medical product, including surgical instruments and devices, has a manufacturer that specifies the product’s instructions for use (IFU). The instructions for product use are non-negotiable; every operator must respect them when using the product.
A typical IFU document of a surgical instrument (PDF) contains the following information:
- General data for the manufacturer and product
- Date of production
- Purpose and indication
- Contraindications
- Materials used
- Sterilization, cleaning, and disinfection instructions
- Inspection, storage, and transportation instructions
- Warnings, cautions, and precautions
- Further explanations on labeling symbols
For instance, a Gelpi retractor requires specific handling to maintain its self-retaining mechanism. Improper cleaning can damage the instrument’s spring tension, rendering it ineffective. To ensure the retractor’s functionality, manufacturers specify its exact cleaning temperatures, approved detergents, and sterilization cycles unique to its specific metal composition.
Ignoring manufacturer guidelines and instructions can result in instrument damage (wear, corrosion, loss of function) and staff and patient harm.
Ignoring signs of damage or wear
Nothing lasts forever and this applies to surgical instruments, too. Any reusable surgical instrument will degrade with use over time despite undergoing regular and appropriate maintenance cycles.
The sterilization team and operating room staff must recognize and promptly address instrument damage or wear, whether it was caused by frequent use or mishandling. Surgical instruments that contain pitting, friction spaces, cracks, or crevices do not work correctly during surgery. Moreover, their damaged regions are hard to clean; as such, they may serve as gathering spots for pathogenic microorganisms.
An intentional or unintentional failure to notice instrument damage or wear is a major mistake that can lead to failed surgeries, tissue damage, and worse patient outcomes.
Incorrect documentation
The documentation of an instrument’s maintenance cycles serves as a critical medical record tracking the entire lifecycle of surgical tools. This documentation typically includes details about cleaning, sterilization, storage, and use. Proper documentation protects the patient by providing a transparent trail of an instrument’s condition.
Incorrect or incomplete documentation can lead to instrument misuse, an inability to trace contamination sources, and an increased risk of surgical site infections.
Medical facilities can prevent documentation mistakes by implementing standardized record-keeping protocols. They can organize staff training courses focusing on what is necessary for precise documentation and employ digital tracking systems and internal audits to verify documentation accuracy and completeness.
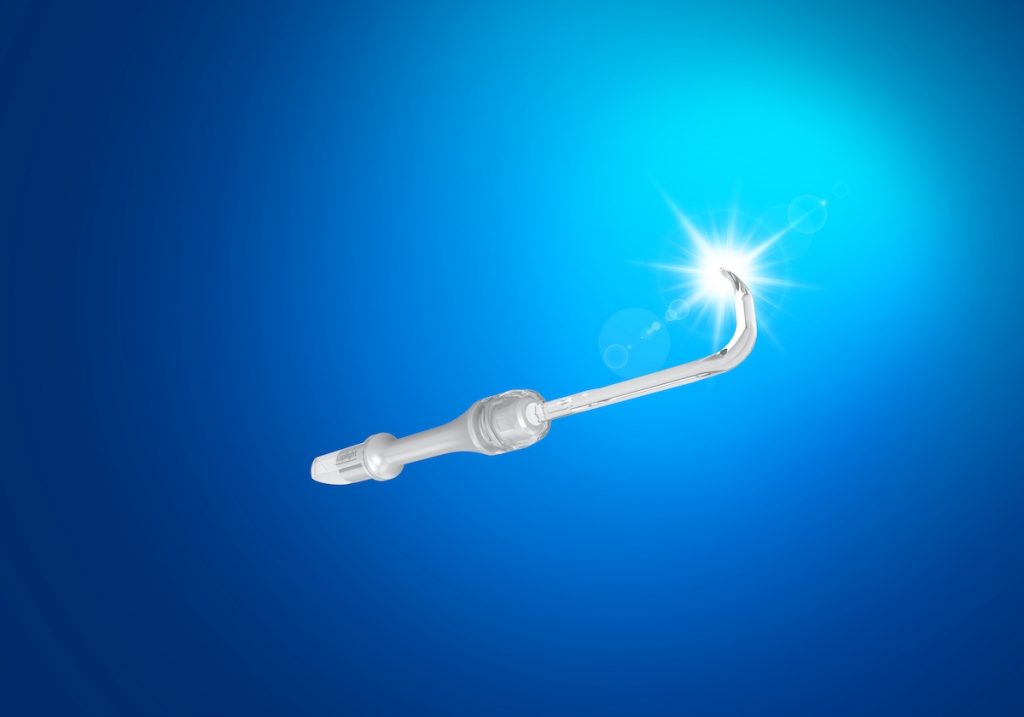
A safe, disposable retractor
The Yasui koplight™, made with disposable plastic blades, is a safe, lightweight, easy-to-maintain, cordless and handheld retractor. With made-in-Japan quality, surgeons and OR staff may find this to be one of the easiest instruments to maintain. Learn more about the koplight™ here.