The mechanical force needed for retractors to allow adequate retraction often significantly compresses tissues. Excessive compressive force during retraction has been shown to cause irritation and damage to muscles, nerves, vasculature, and internal organs. It can be a matter of technique or the device itself.
This article will overview the common retractor-associated tissue traumas across different surgical specialties, as well as how the problem can be lessened, such as through the use of handheld retractors.
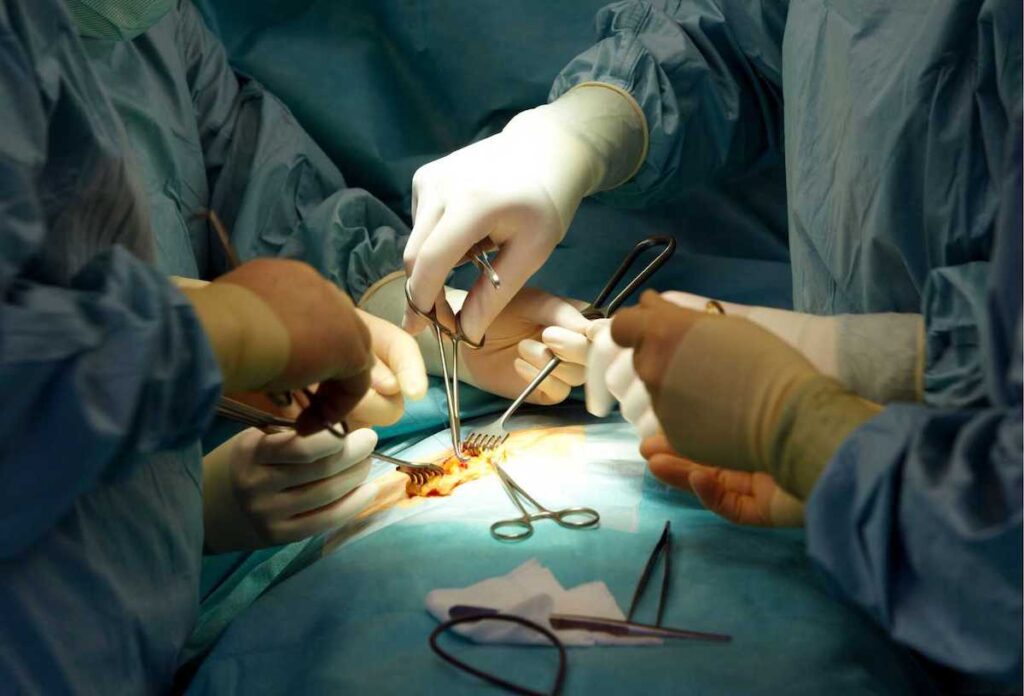
In surgery, retractors are used to displace tissues and organs away from the surgical area, allowing access to the inner, deeper layers.
Retractor-related organ trauma refers to temporary or permanent injury caused by the intraoperative retraction of an organ. Often these injuries are missed, and they resolve on their own, but rarely they may cause significant post-operative complications.
Most commonly, retractor-related organ trauma occurs in the liver; both during laparoscopic and open abdominal gastrointestinal surgeries using handheld and self-retaining retractors. Reports of retractor-related brain and bowel trauma can also be found.
The commonly used Senn tissue retractor is one example of a handheld skin hook. This L-shaped instrument can have two or three curved prongs with either sharp or blunt tips. It provides delicate retraction in plastic, hand, vascular, and thyroid surgeries, and other procedures involving soft tissue and skin.
The Wiener skin hook is another common handheld hook-type skin retractor. This instrument has a single hook and is used for most skin and soft tissue retraction purposes. Other skin retractors include the larger Frazer and Freer skin hooks, and the smaller Tyrell skin hook, used to retract delicate flaps.
Liver trauma
The liver parenchyma is very fragile and non-elastic. This makes it prone to trauma from retractors. Retractor-related liver injury can be classified into traumatic parenchymal tears and parenchymal congestion injuries.
Hepatic parenchymal tears represent direct liver injuries from sharp retractor blade edges during forceful retraction. These tears rupture bile ducts and blood vessels and form one or more cavities filled with bile and blood. Most often, this occurrence is identified intraoperatively and only causes self-limiting bleeding. However, in rare circumstances, it may go unnoticed and form a subcapsular hematoma. These may rupture postoperatively and cause significant bleeding.
Hepatic parenchymal congestion injuries result from prolonged, static compression of the liver parenchyma or vascular structures by the retractor blade. Most often, these pressure-related injuries are temporary and only cause transient asymptomatic elevation of liver enzymes. A condition termed “retraction transaminitis.”
However, prolonged compression of large segments of the liver or major vessels can be severe enough to cause ischemic changes or delayed venous infarctions. Very rarely, these infarcted segments may be complicated by bile leaks, secondary infections forming well-formed abscess cavities, and liver necrosis with septic shock.
There are several ways in which retractor-related liver trauma can be mitigated:
Use of protective packs and modern padded retractor blades can reduce liver injury.
Research has shown that enlarged, fatty, and/or fragile liver lobes are more prone to retractor-related trauma. In these cases, it may be better to use handheld retractors. These instruments allow for modulation of retraction pressure based on anatomic position, reducing the risk of injury.
During prolonged operations, liver damage may be avoided by repositioning of retractor blades. This prevents the concentration of significant pressure in a single area of the liver. For this, handheld retractors, allowing easy and precise repositioning at regular intervals may be beneficial.
Handheld organ retractors are commonly used in open abdominal and thoracic surgeries. These instruments are specially designed with wide, blunt blades and curved tips that can safely and atraumatically retract internal organs. They also shield delicate organ tissues from other sharp instruments.
Intestinal trauma
Retractor-related intestinal trauma is an uncommon complication of gastrointestinal, hepatobiliary, and major vascular surgeries.
Intestinal injuries due to retractors are thought to occur due to either direct injury from the retractor blades or from bowel ischemia due to retractor-related trauma to collateral intestinal vessels.
In addition to applying the concepts mentioned above for liver trauma prevention, the following suggestions may reduce retractor-related intestinal trauma:
Certain patient characteristics predispose to intestinal trauma. These characteristics can include immunosuppression, a history of diverticulitis, and/or a high body mass index. In these patients, classic handheld retractors may be safer. As mentioned, using these instruments allows for precise modulation of retraction pressure.
Brain trauma
Retractor-related brain trauma is not uncommon in the medical literature. Most research indicates that retractor-injury-related postoperative deficits in up to 29% of cases.
During neurosurgery, gaining sufficient access and visualization of brain tumors, aneurysms, hematomas, and other malformations is paramount. Such access and visualization are often achieved using thin metal blades that retract normal brain parenchyma. Unfortunately, pushing apart normal brain tissue may cause retractor-related brain trauma.
Such trauma can result from direct parenchymal injury or focal pressure, causing deformation and/or occlusion of blood vessels with subsequent edema and impaired oxygen delivery to cells.
Over the years, multiple methods have been used to reduce retractor-related brain trauma. These include:
Eliminating uncontrolled retractor movement and improved stability through the use of table-mounted, self-retaining, stereotactically placed retractors and head fixation devices.
Using rounded-edged and malleable retractor blades that cause less damage to cortical vessels than flat, sharp-edged retractor blades.
Using stereotactically guided cylindrical retractors that minimize focal pressure-related damage by evenly distributing pressure to surrounding brain tissues.
Developing and using brain retraction pressure monitoring systems that provide visual or tactile feedback.
Using “chemical brain retraction” –specialized anesthetic techniques and medications that decrease brain volume and intracranial pressure. This allows access to the operating site without the need for excessive pressure under the surgical retractors.
Retractor-related musculoskeletal trauma is well documented. These types of injuries are especially common following thoracotomies and sternotomies done during cardiothoracic surgeries.

Self-retaining ratchet retractors – such as the Finochietto, Ankeney, DeBakey, and Cooley – used during sternotomies and thoracotomies exert great force on the thoracic cage. This force is often the cause of trauma.
Rib fracture is the most common retractor-related musculoskeletal injury following cardiothoracic procedures. Rib fractures are often accompanied by damage to the intercostal nerves. This injury bundle often causes impaired respiratory function and pain, both acute and chronic.
Surprisingly only a handful of studies have evaluated how this type of injury can be mitigated. One study offers recommendations on reducing musculoskeletal tissue trauma during retraction using Finochietto-style retractors:
- Slow, gradual opening of the chest retractor helps reduce the incidence of rib fractures.
- Stabilize the retractor blade with one hand while rotating the crank.
- Take pauses when cranking the retractor open. This allows for force relaxation, decreasing the maximum force of retraction.
- Use padded retractor blades.
- Avoid placing the proximal edges of the blades closer to the end of the incision that is nearest the rack.
- Avoid or minimize all unnecessary movements of the retractor, such as lifting, rotating, or pushing. These small changes can produce large changes in the forces applied to the tissue. This increases the risk of tissue damage.
- If available, use force-controlled retraction. This has been shown to significantly reduce retraction forces and, in turn, reduce tissue damage.
Direct and indirect nerve injury due to retractor-associated trauma is a known complication of several surgeries. Improperly placed retractors can compress nerves causing direct injury. They may also indirectly injure nerves by interrupting their blood supply.
One common example of retractor-related nerve trauma is femoral and obturator neuropathy following total hip replacement (THR). An estimated 0.17% to 3.7% of THR procedures are associated with nerve damage.
It’s hypothesized that retractors placed around the acetabulum during THR are major culprits of nerve injury. When these retractors slip during placement or become displaced due to intraoperative movement, they can compress the femoral and obturator nerves.
Nerve damage may also occur during abdominal procedures. Direct pressure from the metal blades of both handheld and self-retaining abdominal wall retractors can damage the femoral nerve. Although, one study that evaluated the incidence of femoral neuropathy after abdominal hysterectomy found that the incidence of nerve damage was higher with self-retaining systems (7.45%) than with handheld devices (0.7%).
These recommendations may reduce the risk of retractor-associated nerve injury:
- Use protective packs and padded blades.
- Frequently reposition retractor blades at regular intervals.
- Use shorter and more convex blades for slender patients.
- Carefully and precisely place self-retaining retractors.
- Prevent excessive shifting and frequent movement of retractors.
Thermal skin burns are yet another one of retractor-related traumas. This type of injury is specifically associated with using handheld fiber-optic lighted retractors.
The halogen and xenon light sources used in fiber-optic lighting become very hot. For instance, the distal ends of fiber-optic cables have been shown to reach temperatures up to 239°C (462°F). At these temperatures, human skin can easily be scaled or burned.
Similarly, several steps can be taken to reduce retractor-associated skin injury risk:
Use handheld LED-lighted retractors, such as the Yasui koplight. LED-light sources have high energy efficiency and produce less radiant heat. This translates to less risk of retractor-related thermal skin trauma.
Ensure that fiber-optic cables and cords are not in close direct contact with the skin for a prolonged period of time.
A handheld retractor for greater control (and light)
The Yasui koplight is lightweight and handheld. Its onboard LED lighting in the body and head allows fine control during surgery, with minimal fatigue. Learn about the koplight here, and contact us with specific inquires.